Raising Awareness of Ovarian Cancer
Welcome to the London Gynaecology blog!
We look forward to being able to share our thoughts, comments and ideas about women’s health on a regular basis.
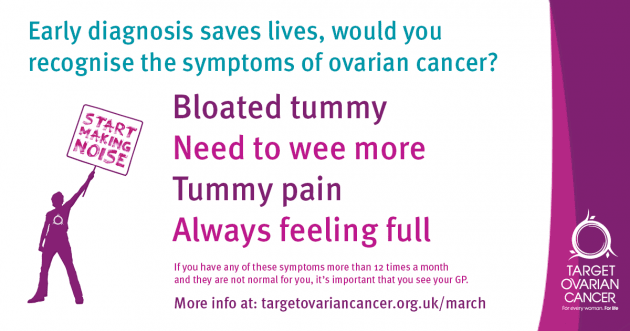
As March is ovarian cancer awareness month it’s natural that we would raise awareness of this disease. Ovarian cancer affects one in 50 women at some stage in their lives, early diagnosis significantly increases the prognosis with chances of surviving ovarian cancer for five years of more increasing from 46% to more than 90%. Therefore creating awareness of this disease and its symptoms is extremely important.
If you want to help raise awareness of ovarian cancer, please share this blog post using the buttons at the end of the article.
What is ovarian cancer? What is the risk I’ll get ovarian cancer?
Ovarian cancer starts in the ovaries and often causes very minimal symptoms in the early stages. It is known to progress quickly and hence early detection is important. Lifetime risk of getting ovarian cancer for women is around 1 in 50 (2%).
Family history of ovarian cancer in one first degree relative would be associated with doubling of the risk (1 in 25 or 4%). BRCA 1&2 genes are associated with high risk of ovarian cancer (up to 50%).
What are the symptoms?
Ovarian cancer is notorious for causing very minimal symptoms in the early stages. Hence high index of suspicion and being aware of symptoms is important. Ovarian cancer commonly occurs after menopause (after 50 years of age) and symptoms can be non-specific such as:
- Abdominal distension and bloating
- New onset of pelvic pain
- Nausea and fullness
- Urinary frequency
- Loss of appetite and weight
- Lower abdominal lump
Please see your GP urgently if you are concerned and he/she will be able to arrange appropriate tests or referral on an urgent basis.
How is ovarian cancer diagnosed?
An ultrasound scan and a blood test (CA125) can often give a provisional diagnosis, but the diagnosis is only confirmed after biopsy (usually after removal of any ovarian lesion). An MRI scan will often give more specific and detailed information before surgery. It also helps in planning the management.
Cervical smear test will NOT detect or rule out ovarian cancer! It is aimed at detecting cervical pre-cancerous changes and is nothing to do with ovaries.
What about screening?
CA125 and ultrasound scan have also been used for screening especially in women at higher risk of developing ovarian cancer. However, these tests can be both falsely positive and negative. Benign ovarian cysts are very common and CA125 is raised in many common conditions such as fibroids and endometriosis. Also, only 50% of stage 1 and 80% of all ovarian cancer will have raised CA125. Even if we do annual screening, there is a chance of developing disease in the interim.
We can discuss and offer screening for ovarian problems. Please visit www.london-gynaecology.com
What type of ovarian cancer, fallopian tube cancer, or peritoneal cancer do I have?
This information can often be obtained after an MRI scan or operation and biopsy (histology).
What are the treatment options for ovarian cancer?
Surgery to remove as much of the tumour and disease as possible is often the first option (though not always). If there is evidence or suspicion of spread outside the ovaries, additional chemotherapy may be recommended.
I’ve been diagnosed with ovarian cancer. What do I need to know?
Your doctor and CNS (Clinical Nurse Specialist) would be the first point of call as they would be able to provide information specific to your circumstances. Not all the information that you read online or in leaflets will apply to you and you must not draw any conclusions unless discussed with your team. You can get general information on websites such as www.ovacome.org.uk or www.cancerresearchuk.org or www.macmillan.org.uk.
What are the chances of beating ovarian cancer?
This often depends on your individual circumstances (such as age, medical condition, type and stage of ovarian cancer and response to treatment) and your doctor will be able to provide more specific information. It is important to ask questions (take somebody with you for consultations) and if there are no direct answers, you can always find out about best and worst possible scenarios.
What should I do to protect myself from ovarian cancer?
We recommend a “MOT@50” (well-woman check at 50years of age) which your GP can organise or we will be happy to arrange. Please visit www.london-gynaecology.com for more information.



