News
-
26th June 2025 | Posted by Alisha Esmail
When should I see a Private GP?
Why would I see a private GP instead of my NHS GP?
- Seeing a private GP can offer you more time, flexibility, and faster access. Appointments are typically longer, more in-depth, and can be scheduled at a time that suits you – often the same day. It’s a good option if you want to avoid waiting lists, need more personalised care, or have concerns you’d like to explore in more detail.
Can I get a same-day appointment?
- Yes. In most cases, we can offer same-day appointments. At busier times, appointments are usually available within 24 hours. This means you can be seen quickly and start any necessary treatment or investigations without delay.
What kind of issues can a private GP help with?
Our GPs are experienced in a wide range of health concerns, including:
- Women’s health and gynaecological symptoms
- Menstrual problems and hormone-related concerns
- Menopause management
- Contraception and sexual health
- General health checks and preventive care
- Minor illnesses or infections needing prompt treatment
They also offer Well Woman checks and can refer directly to our consultants if specialist input is needed.
Can a private GP help with the same things as my NHS GP?
- Yes. Our private GPs can help with any general health issue you would usually take to your NHS GP. This includes everything from infections, skin problems, and fatigue to ongoing conditions like asthma, anxiety, or high blood pressure. They can also see and review you for mental health conditions. You don’t need a specific women’s health concern to book an appointment.
Is it worth seeing a GP for just one concern?
- Absolutely. Even if it’s something simple – like a suspected infection, a concern about your period, or a request for advice – a private GP can help you get answers quickly, and if necessary, refer you for tests or specialist care right away.
Can the GP refer me to a specialist?
- Yes. One of the benefits of seeing a private GP at London Gynaecology is direct access to in-house diagnostics and consultants. If you need an ultrasound, blood tests, or a consultation with a specialist, your GP can arrange this for you with minimal delay. They can also provide referral letters for other specialists if you have healthcare insurance.
Can your private GP refer me for scans, blood tests, or X-rays?
Yes. Our private GPs can arrange a full range of investigations quickly and efficiently. This includes:
- Blood tests (with fast turnaround times)
- Ultrasound scans
- X-rays
- MRI and CT scans
- Smear tests and other diagnostics
Because we work closely with leading diagnostic centres and in-house specialists, these can usually be arranged within days – or even same-day in urgent cases. You’ll also get clear, prompt follow-up and support with any results or next steps.
Do I need a referral?
No referral is needed. You can book directly with us – online, by phone, or in person. Whether it’s for a specific concern or a general check-up, we’re here to help.
How long are appointments?
Appointments are typically 30 minutes, which is significantly longer than standard NHS GP slots. This gives you time to talk through your concerns in detail, without feeling rushed. Any follow-up appointments needed for the same problem are usually 15 minutes.
Can I get prescriptions?
Yes. We can issue private prescriptions during your appointment, and many medications can be collected the same day from a local pharmacy. You could also opt for a home delivery service too. If ongoing treatment is needed, we’ll discuss the best and most convenient options with you.
I’m registered with an NHS GP, can i still see a private GP?
Yes. Seeing a private GP doesn’t affect your NHS registration in any way. Many of our patients use us for faster access, specialist referrals, or second opinions while remaining registered with their NHS GP. We’re also happy to provide a summary letter for your GP, updating them of any changes.
Can my medical insurance cover a private GP appointment?
Some health insurance policies do cover private GP appointments, but it depends on your provider and your specific policy. We recommend that you check directly with your insurer before booking, to confirm whether your consultation and any tests or referrals will be reimbursed. We can provide you with a detailed invoice or receipt if you wish to claim back the cost through your insurance.
Choosing to see one of our private GPs offers greater flexibility, convenience, and personalised care – without long waits or rushed appointments. Whether you’re seeking support for a specific concern or simply want a more thorough, proactive approach to your health, our experienced GPs are here to help. You don’t need a referral, and appointments can often be made the same day. If you’re considering private healthcare, this could be a simple investment in your health toward feeling better, faster.
Click on the Our Team tab to meet our experienced in-house GPs!
-
5th June 2025 | Posted by Alisha Esmail
HPV & Cervical Screening: FAQs answered by the experts
1. I feel absolutely fine – do I really need a smear test?
Yes, 100%. Cervical cancer can develop without any obvious symptoms, which is why cervical screening (also called a smear test) is so important. It can detect changes before they become anything serious. A quick test today could genuinely save your life.
The cervix is the lower part of your womb (uterus), sitting at the top of your vagina. It acts like a gateway between the two.
While cervical cancer is more common in women aged 30-45, it can affect people in their 20s too. That’s why starting screening is crucial – even if you feel perfectly well.
2. At what age should I start going for smear tests?
In the NHS, you’ll be invited for your first HPV screening at age 25. From there, it’s now every 5 years, up to 64 years, but you might be called back sooner if you get a positive HPV result.
At London Gynaecology, we often recommend more frequent screening to be thorough, especially if your medical history or previous results suggest it’s needed. Your care plan is always tailored to you.
3. What is HPV and why does it matter?
HPV (Human Papillomavirus) is a super common virus – around 8 in 10 people will have it at some point. It’s picked up through skin-to-skin contact during sex. You don’t need full penetrative sex to get it and it can be picked up from a partner even if they have no symptoms. Most types clear up on their own without any issues, but some high-risk types can lead to abnormal cells on the cervix, which – if left untreated – can develop into cervical cancer. Over 99% of cervical cancers are caused by HPV.
That’s why your initial screening test checks for HPV. Catching it early means we can monitor or treat any changes long before they become anything serious. If HPV is present, you will then need a smear test to check the cervical cells.
4. What actually happens during a smear test?
The whole thing usually takes just a few minutes. Here’s what to expect:
- You’ll lie on an exam bed, usually with a paper sheet over your lower half
- A nurse or doctor will gently insert a small speculum to see your cervix
- They’ll use a soft brush to collect a sample – this might feel odd, but it’s quick and usually not painful
That’s it! You can go straight back to your day.
We’ll always explain what’s happening and check in with you throughout. If you’re feeling nervous, just let us know – we’re here to help you feel at ease.
5. What if I am nervous or embarrassed?
Totally understandable – and you’re not alone. We’re here to help you feel safe and supported. We have:
- Female clinicians available
- Calm, private, and respectful environments
- Trauma-informed care for anyone who’s had previous difficult experiences
You’re always in control – and we’ll go at your pace.
Looking for ways to make your smear more comfortable? Check out our in-house tips here. Cervical Screening Awareness and Recommendations: How To Make Your Smear Test More Comfortable – London Gynaecology
6. What if my smear test shows something abnormal?
First: try not to panic. Most abnormal results don’t mean cancer – but they do mean we’ll want to keep an eye on things.
You might be referred for a colposcopy with one of our Consultants – this is similar to a smear test but just a closer look at your cervix using a special microscope. It’s done in our clinic, takes around 15–20 minutes, and helps us understand what’s going on.
If needed, we’ll talk you through treatment and follow-up options.
We’re here every step of the way.
7. Do I already have symptoms of cervical cancer?
In the early stages, there often aren’t any. But it’s important to look out for:
- Bleeding between periods or after sex
- Pain during or after sex
- Unusual vaginal discharge
- Persistent pelvic or lower back pain
If you notice any of these, don’t wait – get it checked, even if your last smear was normal.
8. What are the new home HPV kits?
They’re self-sampling kits offered by the NHS as part of a trial programme. Instead of going to a clinic, you use a small swab to take a sample from your vagina at home, then post it back for testing. This only tests for HPV, and doesn’t test for cellular changes. If your test is positive, you will then be called for a smear test.
At London Gynaecology, we recommend having a full HPV and smear check for a complete and thorough check.
9. What cervical health services do you offer?
At London Gynaecology, we offer:
✔️ Cervical screenings (smear tests)
✔️ HPV testing (with detailed results of high-risk and low-risk types)
✔️ Colposcopy and follow-up treatment (if needed)
✔️ Expert care from GPs and gynaecologists, all under one roof10. How do I book an appointment?
- Call us on 0207 1011 700
- Book online
- Or drop in – we’d be happy to help!
Sources & References
- HPV prevalence: “Epidemiology and Natural History of Human Papillomavirus Infections in the Female Genital Tract” – PubMed (PMID: 24350604)
- Most HPV infections clear on their own: “Human papillomavirus infections: epidemiology, pathogenesis, and prevention” – PubMed (PMID: 15142639)
- Cervical cancer age range: Cervical cancer incidence by age – Cancer Research UK
- Cervical screening programme details (UK): NHS Cervical Screening Programme – NHS England
- Colposcopy guidance: NICE Guidelines on Colposcopy and Management of Abnormal Cervical Cytology – NICE UK
- Symptoms of cervical cancer: Cervical Cancer Symptoms – Cancer Research UK
-
3rd March 2025 | Posted by Geoff Bamber
17 Questions About Vaginas and Sexual Health
Many questions remain unanswered or are too sensitive or embarrassing to ask during a gynaecology appointment. Miss Aref-Adib spoke with Stylist to address some of the common concerns that many patients think about but are too afraid to bring up. With over half a million people in the UK waiting for a gynaecology appointment, there is ample opportunity for unanswered questions to arise.
Some of the questions addressed include:
– Is penetrative sex ever going to feel as good after I’ve had a baby?
– My discharge seems to be bleaching my underwear – is that normal?
– I feel I’ve got too much labia skin. What’s a ‘normal’ size, and at what point should I consider surgery?
– How has being a gynaecologist shaped the way you view your own vagina and vulva?
– What’s the coolest thing about vaginas people don’t know?You can read the full article, From post-baby sex to smells and UTIs: 17 questions about vaginas and sexual health that you’re too embarrassed to ask – answered by gynaecologists, here.
If you have any questions you’d like answered or need further information on a specific treatment, feel free to contact us.
-
27th February 2025 | Posted by Geoff Bamber
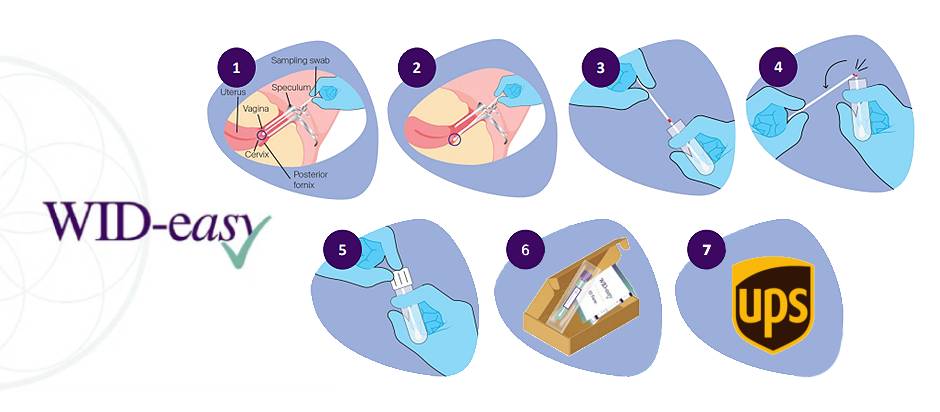
The WID-Easy Test – An Innovative Test for Post Menopausal Bleeding
London Gynaecology will be offering an innovative test which saves several patients from having to undergo invasive procedures for a diagnosis. WID-easy is a genetic test for people suffering from abnormal uterine bleeding during or after menopause.
How is the WID-easy test carried out? How does it work?
Your clinician will take a sample from your vagina and behind your cervix, similar to a PAP smear test, and send it to the lab for analysis. Samples are collected before a transvaginal ultrasound and the overall procedure is simple. WID-easy measures chemical modifications (specifically the methylation levels of DNA in the GYPC and ZSCAN12 genes) of your DNA from your cervix and womb which indicates the presence or absence of cancer cells.
The Benefits
The WID-easy test saves many patients from having to undergo invasive surgery to diagnose whether cancer is the cause of the bleeding. It assists in assessing the urgency of treatment and identifying the appropriate type of treatment needed. WID-easy helps you make informed decisions about your next steps in care, while helping you avoid unnecessary invasive procedures.
- Accurate – results have shown unnecessary follow-up procedures to be reduced by over 90% without missing cancers.
- Rapid – it has been designed for quick analysis, providing fast results within days.
- Simple – the cervical and vaginal swab sample collection is minimally invasive.
WID-easy can be used alongside other diagnostic procedures such as transvaginal ultrasounds however it should be conducted before applying lubricant and taking samples for tests like a PAP smear. It can also simplify diagnosis for women with fibroids or a high BMI.
The WID-easy Test in 7 Steps

- 1. The swab is inserted into the vagina in the upper vaginal region around the cervix.
- 2. For 2-3 seconds, the swab is slowly rotated 360 degrees.
- 3. It is then placed in an eNAT® tube to the predetermined level.
- 4. The sample is deposited within the break point marked in red.
- 5. The tube is then stored safely in an upright position before being sent to a lab.
- 6. Analysis of the sample is performed by a lab using PCR, similar to a COVID test.
- 7. Results are then sent to London Gynaecology within a few days.
What Is the Cost of a WID-Easy Test?
- The WID-easy test is available to self-pay patients for £450 and is not currently covered by insurance.
- For each test, £20 will be donated to the Eve Appeal.
The WID-easy test was developed by researchers at University College London and the University of Innsbruck, in collaboration with The Eve Appeal, the UK’s largest gynaecological cancer charity. To show our support, we donate to The Eve Appeal for each test used.
Where Can I Find More Information on WID-Easy?
For more information on WID-easy, please visit AGHealth. Please do not hesitate to ask our expert gynaecologists about WID-easy during your next appointment.
-
22nd January 2025 | Posted by Emma Orman
Cervical Screening Awareness and Recommendations: How To Make Your Smear Test More Comfortable
It is extremely important to attend regular cervical screening appointments and to adopt other preventive care such as having the HPV vaccination – both help significantly with cancer prevention.
Cervical screenings – more commonly known as a smear test – can be a painful experience, and we understand that for many women and people with a cervix, the expected discomfort may be discouraging. Our consultants and nurses have helped support thousands of people through this process over the past two decades – here are some tips to make your cervical screening more comfortable:
1. Listen to music or watch TV: Nowadays with smartphones, watching a movie or listening to music or a podcast is easy to do in any location. Take your headphones and your phone and get prepared to zone out. And don’t worry, if you do forget your headphones ask the nurse if she minds you watching or listening anyway.
2. Equipment: Ask, if available, for the nurse to use a plastic speculum or a small speculum. Plastic is often warmer than metal and it’s clear so it’s easier for the nurse to see the cervix and a smaller speculum is more comfortable. They aren’t always available but don’t be afraid to ask.
3. Count from 1 to 100: Paula Radcliffe used to use this strategy towards the end of her marathon and many patients have found it useful. Often the smear is done well before you get to 50.
4. Paracetamol: Take a dose of paracetamol 30 minutes before your smear which will take some of the discomfort away.
5. Numbing gel: If all else fails, ask the nurse to use a small amount of numbing gel. Previously there was a concern that the gel would affect the smear cytology but with liquid based cytology which is used nowadays a small amount of gel will not interfere with the quality.
6. Vaginal oestrogen cream: If you have vaginal dryness symptoms linked to breast feeding or menopause ask for local vaginal oestrogen cream. This can make a smear test much more comfortable and is a very safe treatment. It can be stopped 2 days prior to the smear test. In addition to, or as an alternative to, local oestrogen, using a good pH-balanced vaginal moisturiser several times a week can be very beneficial such as YES vaginal moisturiser.
7. Practicing with a speculum: If you are concerned about the speculum, why not ask your practice nurse if you can try one out at home to get used to the sensation.
8. Communicate: If it feels uncomfortable or you feel worried at any point during your smear, ask the smear taker to stop. We can go at your pace.
9. Relax: Try taking slow and deep breaths which can help to relax your pelvic muscles. Find a technique that works for you – mindfully changing your breathing patterns can improve relaxation which in turn will help to make the appointment smoother and quicker.
10. Ask for specialist care: For anyone who has experience trauma or FGM often referral to a specialist service is best. Your healthcare provider will be able to arrange this for you. It is reasonable to ask for adjustments when you have a cervical screening although many are unaware that their tests can be slightly altered – as highlighted by The Eve Appeal.
In general, there remains a knowledge gap and lack of understanding around what a cervical screening is for and how it can help.People with a cervix aged from 25 to 64 are offered the NHS cervical screening programme in England and routine screening is offered every 3 years up to the age of 49; every 5 years for those from 50 to 64 years old.
The NHS Cervical Screening Programme, England 2023-2024 annual report, published in November 2024 by NHS England, showed:
- Only 63% of 5.12 million individuals invited to book an appointment were tested.
- 31.2% of 25 to 64-year-olds were not screened within the recommended time.
- For the 2023-24 period, there was a 1.8% increase in referrals (approximately 250,000) to colposcopy considering all ages and referral reasons.
Even if you have been vaccinated against HPV or think that you have not seen or experienced any symptoms, it is still important to attend cervical screening appointments.
We encourage anyone whose test is overdue to book their appointment. If you have any questions or need further information, London Gynaecology can help.